Children's Mental Health Statistics 2026 - Key Facts and Trends
As we settle into 2026, the landscape of childhood mental health remains one of the most pressing conversations at the dinner table and in the teacher's lounge. While the initial shocks of the early 2020s have stabilized, the data reveals a complex new reality: while awareness is at an all-time high, access to care struggles to keep up with demand. For parents and educators, understanding these numbers isn't about raising alarm - it's about equipping ourselves with the clarity needed to advocate for the children we love.
Key Takeaways
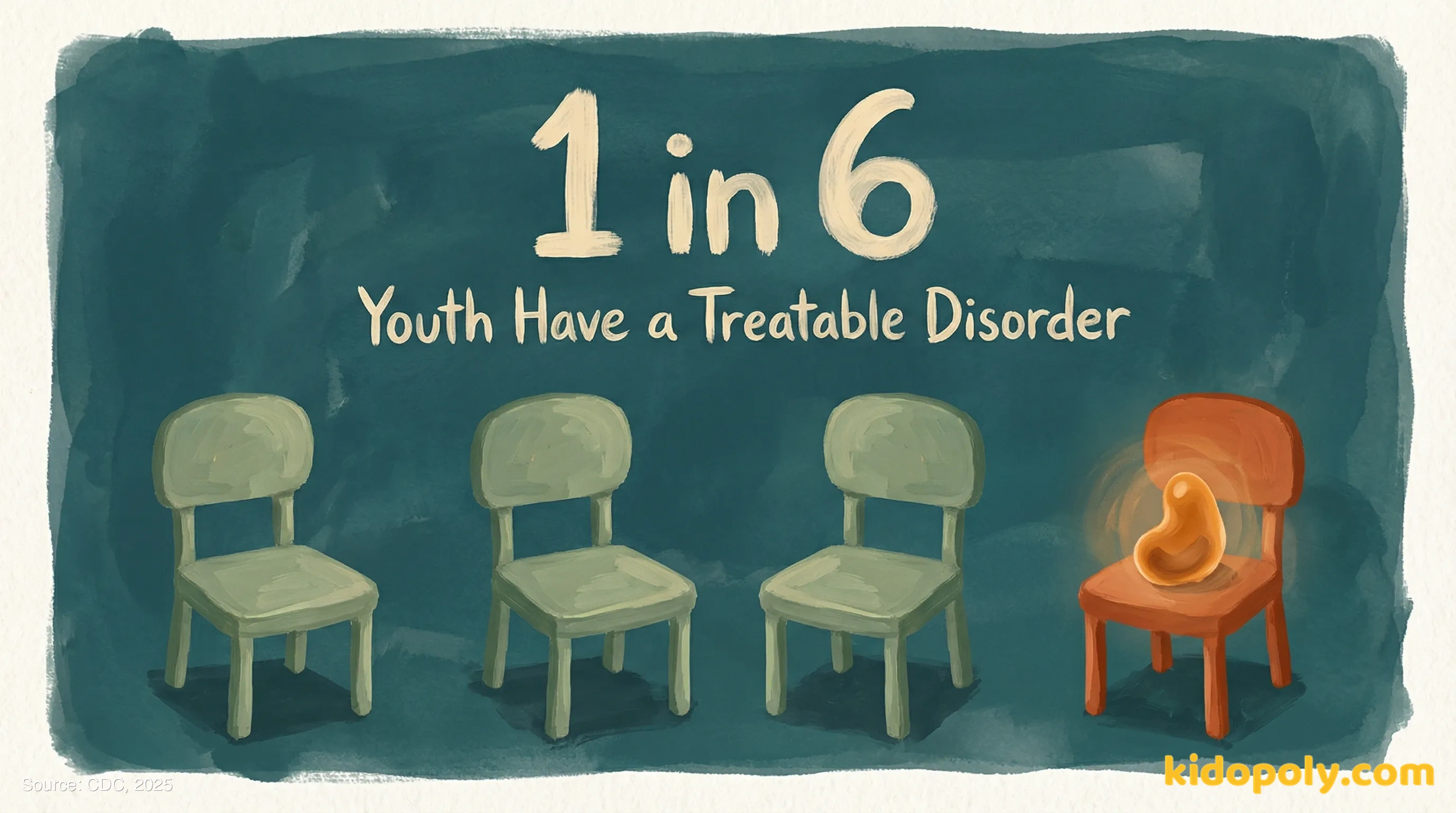
- 1 in 6 U.S. youth aged 6-17 have a treatable mental health disorder (CDC).
- 59.8% of youth with major depression do not receive any mental health treatment (MHA).
- 50% of all lifetime mental health conditions begin by age 14 (WHO).
- Schools provide mental health services for 58% of adolescents who receive care (GMU).
- Emergency department visits for pediatric mental health have risen 14% since 2023 (JAMA).
The Current Landscape: Prevalence and Scope
U.S. youth aged 6-17 with a treatable mental health disorder
This represents approximately 7.7 million children nationwide.
Prevalence of Common Diagnoses in U.S. Children (Ages 3-17)
| Diagnosis | Prevalence Rate | Estimated Count |
|---|---|---|
| ADHD | 9.8% | 6.0 million |
| Anxiety | 9.4% | 5.8 million |
| Behavior Problems | 8.9% | 5.5 million |
| Depression | 4.4% | 2.7 million |
Adolescent Mental Health Trends (2019-2025)
Source: Kaiser Family Foundation (2025)
Access to Care: The Treatment Gap
Youth with major depression who did not receive treatment
Despite rising diagnosis rates, the majority of struggling teens go untreated.
Source: Mental Health America (2026)
Barriers to Mental Health Care for Youth
| Barrier Type | Percentage of Parents Reporting |
|---|---|
| Cost / No Insurance Coverage | 42% |
| No Providers Available/Waitlists | 31% |
| Unsure Where to Go | 18% |
Why is it so hard to find a therapist for my child right now?
Navigating Care Hurdles
- Ask your pediatrician for an 'integrated care' referral, which can bypass some waitlists.
- Check if your employer offers an Employee Assistance Program (EAP) that covers family therapy sessions.
- Contact your school counselor immediately; they often have lists of local providers with current availability.

Global and Regional Perspectives
10-19 year olds globally experiencing a mental disorder
This accounts for 13% of the global burden of disease in this age group.
Source: World Health Organization (2025)
State Rankings: Youth Mental Health Access (Top vs Bottom)
| Rank | State | Access Score |
|---|---|---|
| 1 (Best) | Maine | High Access |
| 10 | Pennsylvania | Moderate Access |
| 51 (Lowest) | Texas | Critical Shortage |
Source: Mental Health America (2026)
The Role of Schools and Communities
Recommended Student-to-Counselor Ratio
Most states still average closer to 385:1, significantly stretching resources.
Source: Project Change Maryland (2026)
Where Youth Receive Mental Health Services
Can schools actually treat mental health conditions?

Hospitalization and Crisis Data
Increase in pediatric mental health ED visits since 2023
Hospitals report growing pressure on emergency departments for behavioral health crises.
Source: JAMA Network Open (2025)
Boarding Times for Psychiatric Patients in EDs
| Wait Time Category | Percentage of Patients |
|---|---|
| Less than 4 hours | 18% |
| 4 to 12 hours | 33% |
| Over 12 hours (Boarding) | 49% |
What should I do if my child is in immediate crisis?
Common Questions from Families
Are girls more affected by depression than boys?
Is social media the main cause of this increase?
At what age do mental health symptoms usually start?
What Families and Educators Can Do
Steps for Home
- Model emotional vocabulary: Name your own feelings (tired, frustrated, hopeful) to normalize the language of mental health.
- Prioritize sleep: Enforce tech-free zones at night, as sleep disruption is a primary aggravator of anxiety symptoms.
- Validate, don't fix: When your child shares a worry, say 'That sounds really hard' before jumping to solutions.
Steps for the Classroom
- Implement 'temperature checks': A simple thumbs-up/thumbs-down check-in at the start of class can help identify students needing support.
- Advocate for ratios: Use the 250:1 recommended counselor ratio data to push administration for better support staff funding.
- Create quiet corners: designate a low-stimulation zone in the classroom for self-regulation breaks.
Sources (10)
- 1. George Mason University Public Health (2026) https://publichealth.gmu.edu/news/2026-02/its-now-easier-ever-navigate-publicly-available-youth-mental-health-data
- 2. Centers for Disease Control and Prevention (2025) https://www.cdc.gov/children-mental-health/data-research/index.html
- 3. Mental Health America (2026) https://mhanational.org/the-state-of-mental-health-in-america/data-rankings/youth-ranking/
- 4. World Health Organization (2025) https://www.who.int/news-room/fact-sheets/detail/adolescent-mental-health
- 5. American Hospital Association (2025) https://www.aha.org/integrating-behavioral-health-pediatric-care-hospital-led-solutions-growing-crisis
- 6. Kaiser Family Foundation (2025) https://www.kff.org/covid-19/roughly-1-in-5-adolescents-report-experiencing-symptoms-of-anxiety-or-depression/
- 7. Project Change Maryland (2026) https://www.projectchangemaryland.org/student-mental-health-statistics-2026-current-rates-risks-and-trends/
- 8. Huntington Psychological Services (2025) https://huntingtonpsych.com/blog/teen-mental-health-statistics
- 9.
- 10. Temple University College of Public Health (2025) https://cph.temple.edu/news/2025/06/depression-rates-us-continue-climb-experts-call-increased-access-care-community-based-interventions
